For athletes, the start of a new season often means long hours of conditioning, refining skills, and building strength. But while training camps and practice schedules are carefully planned, there’s one step many athletes skip: a comprehensive lower body examination and biomechanical screening with a sports medicine podiatrist.
For athletes, the start of a new season often means long hours of conditioning, refining skills, and building strength. But while training camps and practice schedules are carefully planned, there’s one step many athletes skip: a comprehensive lower body examination and biomechanical screening with a sports medicine podiatrist.
Just as you wouldn’t start a season with broken equipment, you shouldn’t head into competition without making sure your feet, ankles, knees, and the mechanics that connect them are functioning correctly. This often-overlooked evaluation can make the difference between a strong, healthy season and one interrupted by preventable injuries.
The Lower Body is the Foundation of Athletic Performance
Your lower body is responsible for some of the most crucial athletic functions, including generating power, absorbing impact, and stabilizing movement to maintain balance and agility in nearly every sport. From sprinting down a track to pivoting on the court or cutting across a turf field, athletic performance depends on efficient lower-body mechanics.
Even seemingly minor misalignments in the feet, ankles, or knees can create a chain reaction upward, affecting the hips, back, and overall movement efficiency. Over time, those small inefficiencies increase injury risk and drain energy that could otherwise fuel performance.
A preseason podiatric exam goes far beyond checking for pain or past injuries. It provides a detailed look at alignment, biomechanics, flexibility, strength, and footwear supports critical components of both injury prevention and performance optimization.
Identifying Biomechanical Imbalances
Most athletes have subtle differences in foot structure, leg length, or muscle strength. While these may not cause problems at rest, the repetitive demands of training and competition can magnify them, leading to overuse injuries.
A sports medicine podiatrist can detect issues such as overpronation (excessive inward rolling of the foot), supination (excessive outward rolling), or abnormal gait mechanics that put additional stress on the joints. Addressing these imbalances with corrective exercises, orthotics, or footwear adjustments early on prevents them from escalating into season-ending problems. 
Overuse Prevention
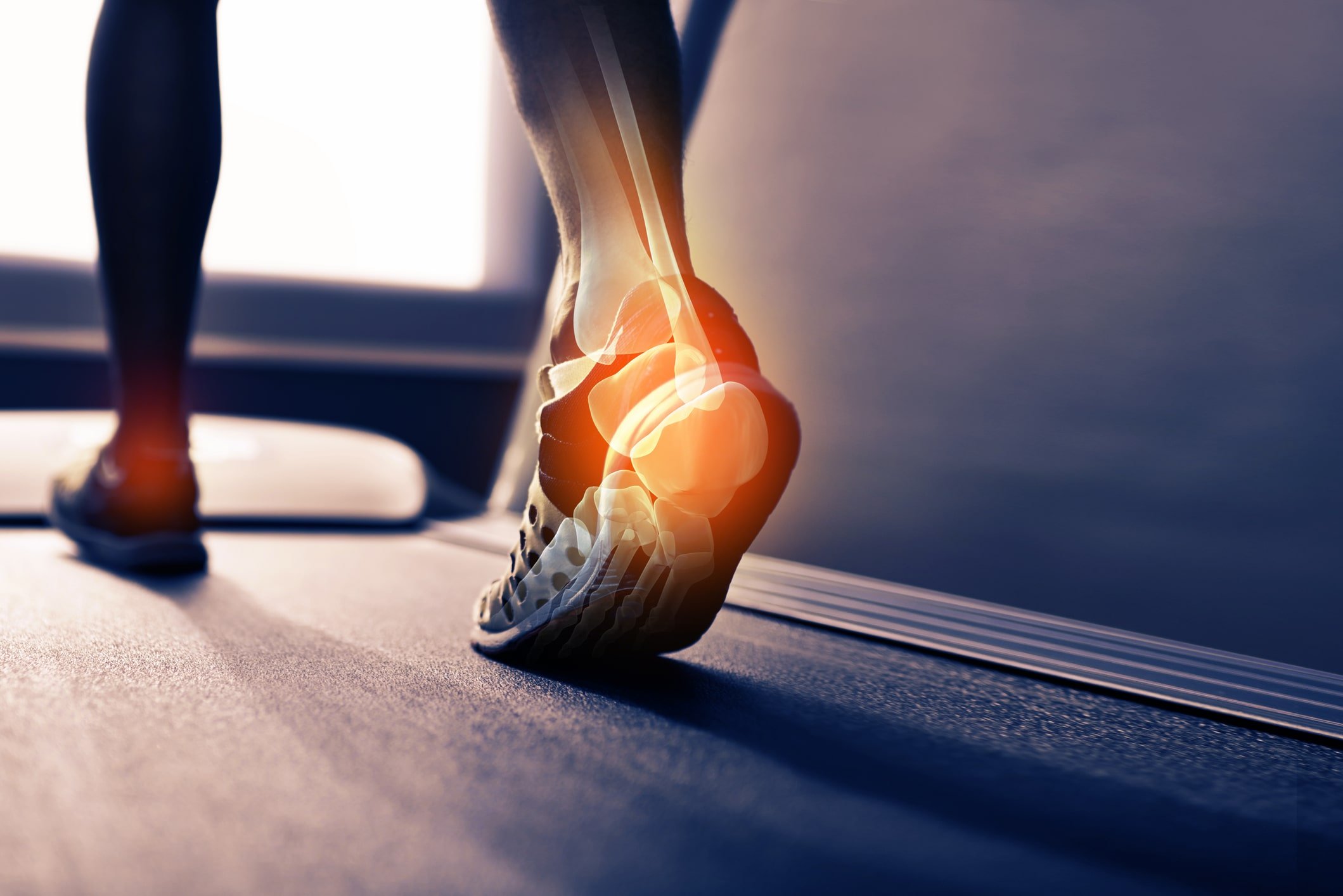
Sports place repetitive stress on the lower body. Without proper support, athletes are more likely to develop conditions such as shin splints, plantar fasciitis, Achilles tendinitis, or even stress fractures.
A preseason exam acts as a proactive safeguard, identifying risk factors before they turn into pain or injury. It’s far easier—and far less disruptive—to prevent injuries than it is to treat them after they’ve sidelined you.
Footwear Optimization
Athletic shoes are not all created equal. Even within the same sport, differences in foot structure, playing surface, and exercise load can significantly affect footwear needs.
Sports medicine podiatrists help athletes select proper footwear and can fine-tune support with custom orthotics or by suggesting necessary adjustments. Something as simple as replacing improper footwear or adjusting insoles can improve performance and reduce the risk of injury.
Monitoring of Past Injuries
An athlete’s history typically includes past injuries such as sprains, stress fractures, or even surgeries. Even when these injuries appear to be resolved, the body may still compensate with subtle changes in movement that can lead to re-injury. 
Prior to each season, lower body assessments and podiatric screenings ensure that past injuries are fully rehabilitated and that movement patterns are stable enough to handle high levels of extreme activity.
Performance Enhancement
While preventing injuries is essential, enhancing performance is equally important. When the lower body moves efficiently, energy is conserved, stride patterns are smoother, and explosive movements—such as sprints, jumps, and directional changes—become more powerful.
By eliminating small inefficiencies, athletes gain an advantage that can lead to increased performance in both the short term and the long run.
Career Longevity
Sports careers, regardless of the level, rely on consistency and durability. Just one preventable injury can set back weeks or even months of hard work. Incorporating preseason podiatric sports medicine screening and evaluations is not just about performance during the season; it’s an investment in the future.
Just as conditioning strengthens the body and practice sharpens skills, a thorough lower body exam ensures that the foundation of performance is solid. By prioritizing this proactive step, athletes can protect themselves from injury, maximize their performance, and set themselves up for success not only this season but for many more to come. 
When the foundation is solid, athletes can focus on what matters most: playing the game they love with strength, confidence, and resilience.
To schedule your comprehensive biomechanical evaluation, contact us or call our Sports Medicine Podiatry Center and book an appointment at our Marlton, N.J. Sports Medicine Facility or Ridley Park, P.A. Office location with one of our podiatric sports medicine specialists today by calling (610) 522-9200.
 Our feet are the foundation of our body’s movement, and when something is misaligned, it can throw everything off balance. One common but often overlooked structural issue is forefoot varus. If you're dealing with chronic foot pain, ankle instability, or even higher issues in your knees or hips, forefoot varus might be playing a role. Let’s dive into what this condition is, how it presents, and what you can do to treat it.
Our feet are the foundation of our body’s movement, and when something is misaligned, it can throw everything off balance. One common but often overlooked structural issue is forefoot varus. If you're dealing with chronic foot pain, ankle instability, or even higher issues in your knees or hips, forefoot varus might be playing a role. Let’s dive into what this condition is, how it presents, and what you can do to treat it.
 If you've ever felt a nagging ache around your kneecap after a long run, hike, or even just going up and down stairs, you're not alone. This condition, commonly known as runner’s knee, is formally referred to as patellofemoral pain syndrome (PFPS). While it’s frequently associated with athletes, it can affect anyone whose movement patterns put extra stress on the knee joint.
If you've ever felt a nagging ache around your kneecap after a long run, hike, or even just going up and down stairs, you're not alone. This condition, commonly known as runner’s knee, is formally referred to as patellofemoral pain syndrome (PFPS). While it’s frequently associated with athletes, it can affect anyone whose movement patterns put extra stress on the knee joint.
 Torn ACLs are a serious and all-too-common injury, especially among athletes in cutting, pivoting, and jumping sports like soccer, basketball, and football. But what if we told you that many ACL injuries are preventable? At our sports medicine podiatry practice, we take ACL risk seriously and use a comprehensive screening approach that looks at the entire lower body, not just the knee.
Torn ACLs are a serious and all-too-common injury, especially among athletes in cutting, pivoting, and jumping sports like soccer, basketball, and football. But what if we told you that many ACL injuries are preventable? At our sports medicine podiatry practice, we take ACL risk seriously and use a comprehensive screening approach that looks at the entire lower body, not just the knee. If you're reading this, it's likely that your heel pain has become more than just a minor annoyance. Perhaps it's interrupting your workouts, making daily walks uncomfortable, or even causing discomfort first thing in the morning before your feet hit the floor. You’re not alone.
If you're reading this, it's likely that your heel pain has become more than just a minor annoyance. Perhaps it's interrupting your workouts, making daily walks uncomfortable, or even causing discomfort first thing in the morning before your feet hit the floor. You’re not alone.